So, your dentist recommended you for a root canal treatment (RCT) and you are pretty apprehensive about it. You search and read every available information on the internet and are left panic struck and confused.
Well, Don’t Worry- This article will definitely you give a clear idea about RCT.
So let’s start by dispelling a common myth: RCT doesn’t cause pain — it relieves it.
Before telling you about the procedure, let’s brush up the basics of tooth anatomy to understand it better.
Teeth contain four layers:
- Enamel: It covers the outermost layer of the teeth which is hardest and also the most highly mineralized substance in the body. Enamel protects the teeth from decay. It forms a strong barrier that protects the inner layers of the teeth from the effects of acids, plaque, and food and beverages that’s very hot or cold.
- Dentin: Dentin is the second layer of the teeth that is protected by enamel on top. It is a layer of calcified tissue consisting of dentinal tubules that directly communicates with the nerve of your teeth causing sensation to pain.
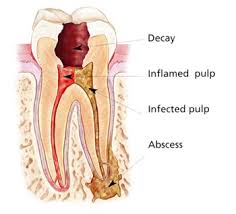
 Pulp: Dental pulp is the central portion of the teeth made up of living connective tissues. It contains nerve fibers and veins. It keeps the organic components of the surrounding mineralized tissue supplied with moisture and nutrients.
Pulp: Dental pulp is the central portion of the teeth made up of living connective tissues. It contains nerve fibers and veins. It keeps the organic components of the surrounding mineralized tissue supplied with moisture and nutrients.- Cementum: It is a hard, calcified layer of tissue that covers only the root of the tooth.
A small decay in enamel or dentin may or may not cause sensitivity or pain. However, when the decay extends up to the pulp, it may cause pain. Pulp is the most sensitive part of the tooth as it is connected to nerves and blood vessels. As and when the pulp is exposed to the outer atmosphere either due to decay or an injury, you are likely to experience tremendous pain.
Root Canal Treatment:
Conservative Endodontic is a branch of dentistry which deals with diagnosis and treatment of dental problems associated with soft tissues inside the tooth.
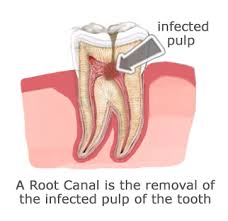
Root canal refers to the natural cavity within the center of the tooth.
Root canal treatment (RCT) is a procedure to repair or save a badly damaged or infected tooth instead of removing it. The goal of this procedure is to save the tooth from pulpal necrosis (disease of pulp). RCT is done both in kids and adults in order to save their tooth from decaying; it stabilizes the tooth and gives it a new life.
Not all tooth decay requires RCT; only if the infection (decay) is too deep your dentist may recommend you this treatment option.
The procedure involves removing the damaged section of the tooth (i.e. the pulp), cleaning and disinfecting the infected portion (the canals), followed by filling and sealing of the tooth and subsequent capping of the infected tooth. Initially after cleaning the canal and filling the canal the tooth is sealed with temporary filling which is soft in consistency.
What Are the Signs That Root Canal Therapy Is Needed?
Signs that you may need a Root Canal Treatment:
- A severe toothache upon chewing or application of pressure
- Prolonged sensitivity to hot and cold temperature
- Discoloration of the tooth
- Swelling and tenderness in nearby gums
- Injury to tooth/Fractured Tooth
Who performs Root Canal Treatment?
While all dentists have received training in the endodontic treatment and can perform most endodontic procedures, in complicated situations you may be referred to an endodontist, a specialist in root canal diagnosis and treatment.
What to expect during the procedure?
Your dentist will examine your teeth and the X-ray and local anesthesia will be administered. Once the tooth and the surrounding tissues are numb, an opening will be made in the crown section of the tooth and small instruments will be used to clear out the canals and shape them for filling. This step may require multiple settings depending on the level of infection. Once the canals have been adequately cleaned and shaped, the canals will then be filled with a polyester synthetic root canal filling and sealer. A temporary filling is then placed to close the opening. Your dentist will remove the temporary filling once the procedure is completed and will seal it with permanent dental cement. The tooth is then reduced in size and crown is placed.
What happens in a root canal treatment?
- Root canal involves a sequence of the following steps:
- Cleaning
- Shaping
- Filling
- Restoration of the tooth
- Crown Placement
Do I need a crown after a root canal?
Front teeth typically do not need a crown after a root canal. However, if the tooth has a lot of decay or is reduced in size and shape than putting a crown will make it aesthetically better.
A crown/cap is very important post RCT, failing to do which may lead to fracture of the treated tooth/teeth. Cap helps you sustain the chewing forces (load) applied on teeth while u chew food, the easiest way to think about whether you need a crown after a root canal is to determine where the tooth is in the mouth. Many studies have shown that a dental crown after a root canal increases the chance of survival of the tooth surviving. Another study conducted showed that only about 1/3 of the molars survive without a crown at 5 years.
- The process of root canal treatment requires drilling or excavation of tooth. Post RCT procedure, a tooth becomes fragile as the process of location of root canals requires lot of tooth structure to be removed.
- In some cases, the decay in the tooth requires an extensive process of tooth removal and thereby makes the tooth weaker. The mastication forces on these teeth can cause fracture of the teeth.
- A dental crown prevents seepage of various oral fluids past a dental restoration. This seepage of fluid can lead to secondary caries and the process is also known as coronal leakage. Coronal leakage leads to RCT failure.
 I already have a crown in my tooth do I still need a new crown?
I already have a crown in my tooth do I still need a new crown?
If the decay is around the edge or the margin of the crown then yes you may need a new. If the decay is under your crown then your dentist might need to remove the crown for a complete accessibility of the decay and a better treatment.
What to expect post-procedure?
Your tooth may feel tender or sensitive for a few days. Your dentist may prescribe you some antibiotics and painkillers to tackle the pain and discomfort. Contact your dentist if your pain lasts for more than a few days. Don’t chew on the affected tooth until symptoms subside and the tooth has been restored as necessary.

